Cost Differences in Cancer Care Across Settings
Cost Differences in Cancer Care Across Settings
In a prior memorandum, we presented evidence documenting the growing share of Medicare oncology volume being billed in the outpatient hospital setting, in comparison to the physician office setting.1 In this report, we present our assessment of the cost consequences to the Medicare program of patients receiving chemotherapy services in physician offices versus hospital outpatient departments on the basis of Medicare data from the years 2009-2011.
In performing this analysis, we have focused on cross-site spending and payment rate differentials that result from differences in the utilization of drugs and services in addition to methodologies employed by Medicare to set payment rates in these two settings.2
Highlights of Our Analyses:
- By a variety of metrics, estimated chemotherapy spending is higher under the Hospital Outpatient Prospective Payment system (OPPS) than corresponding payments in the physician office under the Medicare Physician Fee Schedule (MPFS) for the same set of patients despite lower unit payment rates for drugs in the OPPS during the 2009-2011 period.
- Our comparison of service use rates across settings leads to the conclusion that patients receive more chemotherapy administration sessions on average when treated in the outpatient hospital—and that the dollar value of chemotherapy services used is meaningfully higher in the outpatient hospital.
– Chemotherapy days per beneficiary were about 9 to 12 percent higher in the hospital outpatient department than the physician office setting across the 2009- 2011 period. The difference was 12.3% in 2009, 13.5% in 2010 and 9.6% in 2011.
– On a per beneficiary basis, hospital chemotherapy spending was approximately between 25 to 47 percent higher than physician office chemotherapy spending across the 2009-2011 period. The difference was 25.4% in 2009, 46.8% in 2010 and 33.3% in 2011.
– On a per chemotherapy day basis, hospital chemotherapy spending was 24.3% higher in 2009, 40.1% higher in 2010 and 29.4% higher in 2011 than physician office chemotherapy spending across the 2009-2011 period.
– On a per beneficiary basis, hospital chemotherapy administration spending was 42% higher in 2009, 67.8% higher in 2010 and 51.1% higher in 2011 than physician office chemotherapy administration spending.
- Using only claims data, we cannot determine the extent to which these differences in utilization reflected differences in patient case mix versus differences in facility practice style.
- Re-pricing office chemotherapy administration services using OPPS payment rates creates a volume-weighted payment differential of 19-38% over the 2009-2011 period of our analyses.3 In other words, if all physician office chemotherapy administration services had been paid using OPPS payment rates over the 2009-2011 period, Medicare would have paid 19-38% more for these services.
- Our analysis suggests that a significant portion of the difference in payment rates for chemotherapy administration services between the two sites of service can be attributed to the differing policies adopted by the Congress and CMS that set mechanisms by which OPPS and MPFS payments are updated.
The balance of this report provides further background and details about these conclusions, and the methodology underlying our analyses.
Differences in Utilization and Spending on Cancer Care Between the Hospital Outpatient Department and the Physician Office
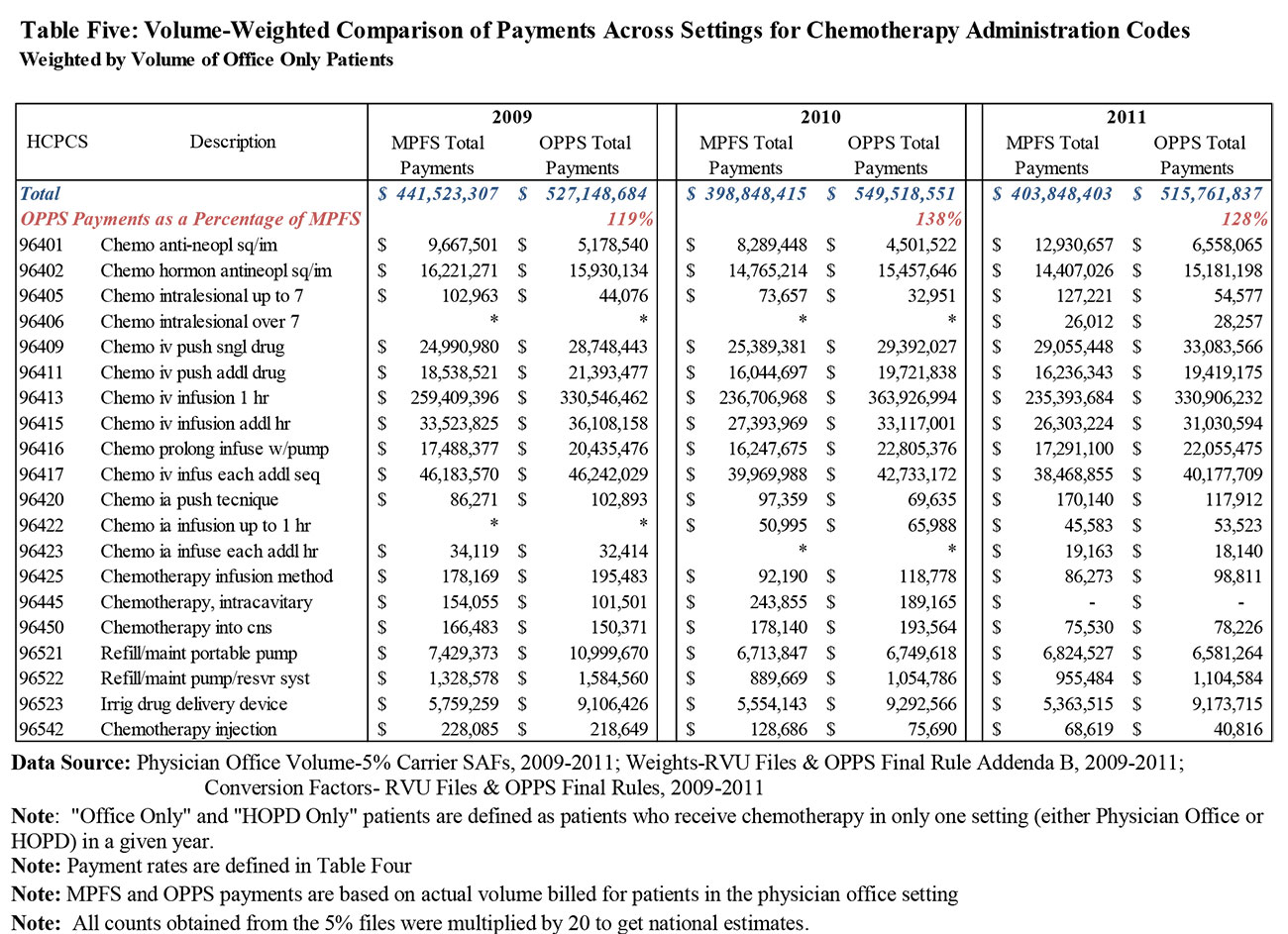
In order to conduct a comparison of the treatment of cancer patients in the OPPS versus the physician office setting, we created a sample of Medicare claims for patients receiving chemotherapy in the year of analysis only in the outpatient hospital (“HOPD Only”) or only in the physician office setting (“Office Only”). The creation of this sample involved the omission of all cancer patients who received chemotherapy in both the Office and HOPD settings in the same year (4.2% of the prior sample). In addition to observing differences in payment rates across settings, we evaluated whether usage patterns differed depending on where patients received chemotherapy. Our analysis derives from a comparison of usage patterns of these two sub-populations.
While we see material differences in use patterns across the office versus the hospital setting, it is important to note that our analysis of claims data does not permit us to parse why usage patterns differ as they do. In particular, we cannot measure any differences associated with beneficiary characteristics (e.g., case mix) or what effects any such differences might have on utilization or spending. In addition, we are aware of anecdotal evidence of transitions from office-based cancer care to hospital outpatient-based cancer care over the past several years based on the acquisition of physician practices by hospital systems. In the case of such an acquisition, there could be a shift from the physician office to the outpatient hospital simply as a consequence of the acquisition, with no differences in patient population.
Illustrative Overview: Service Volumes
The figure that follows compares utilization between the HOPD and physician office for the average beneficiary in our HOPD Only and Office Only samples of Medicare claims
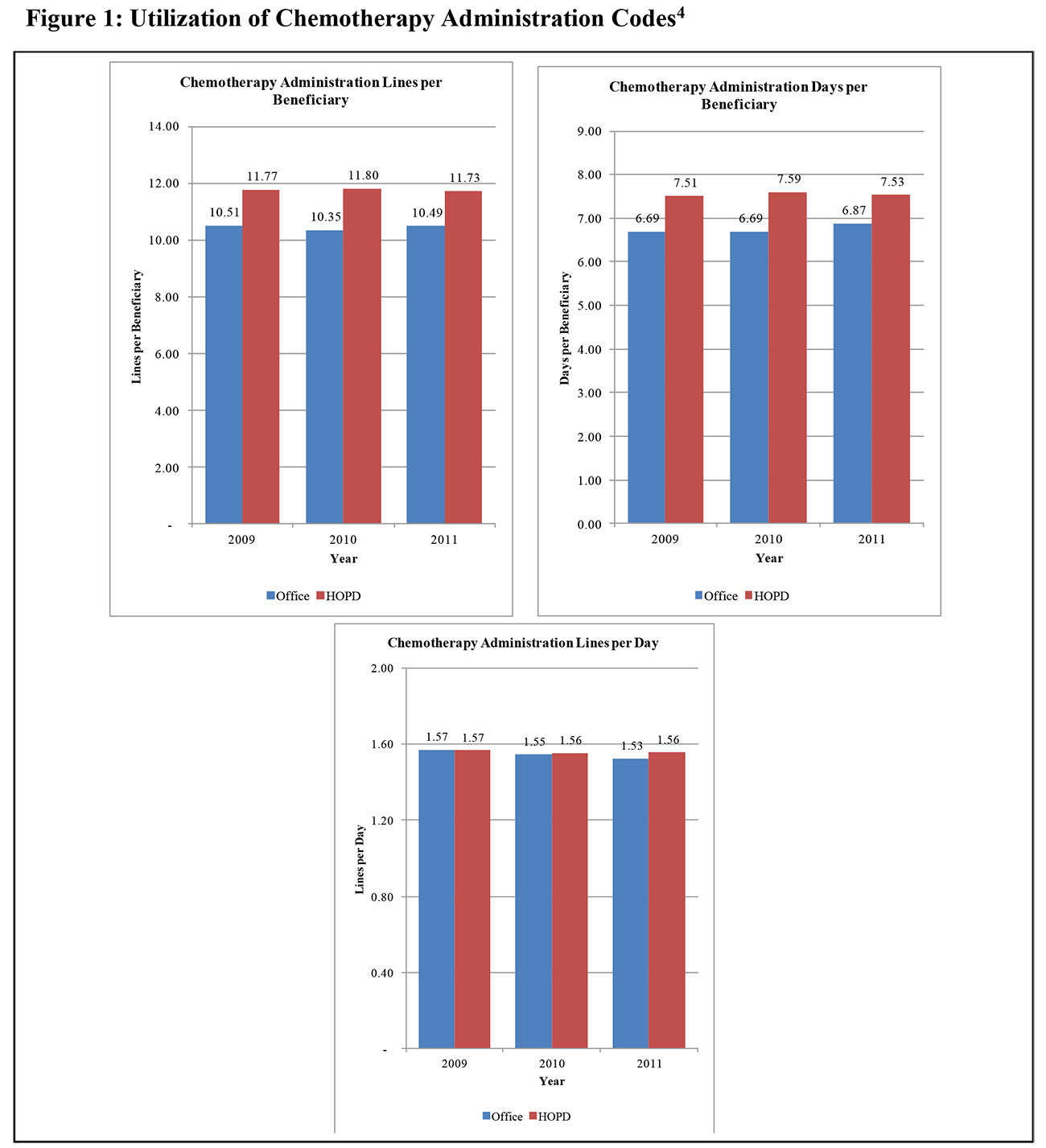
As shown in Figure 1, our comparison of chemotherapy use by Office Only and HOPD Only beneficiaries in these two discrete settings begins with an analysis of the frequency of drug administrations. The figure shows three separate illustrative comparisons:
- These data suggest that the HOPD Only population receives, throughout our period, about one additional day per year of treatment, relative to the days per year observed in the Office Only population.
- The observed difference in chemotherapy administration claim lines per beneficiary further reflects the greater frequency of care received by HOPD only patients.
- However, when we look at the number of discrete drug administration codes billed per day, as measured by the number of discrete service lines recorded on the claims, our data suggest that there may not be a material difference in the number of drug administration codes billed per day of care across settings.
Taken together, these data suggest that, in our period, HOPD Only chemotherapy patients received about a 10-13% higher frequency of drug administration than did Office Only patients. Given the trend pattern, it is unclear whether this spread would be expected to narrow or widen going forward.
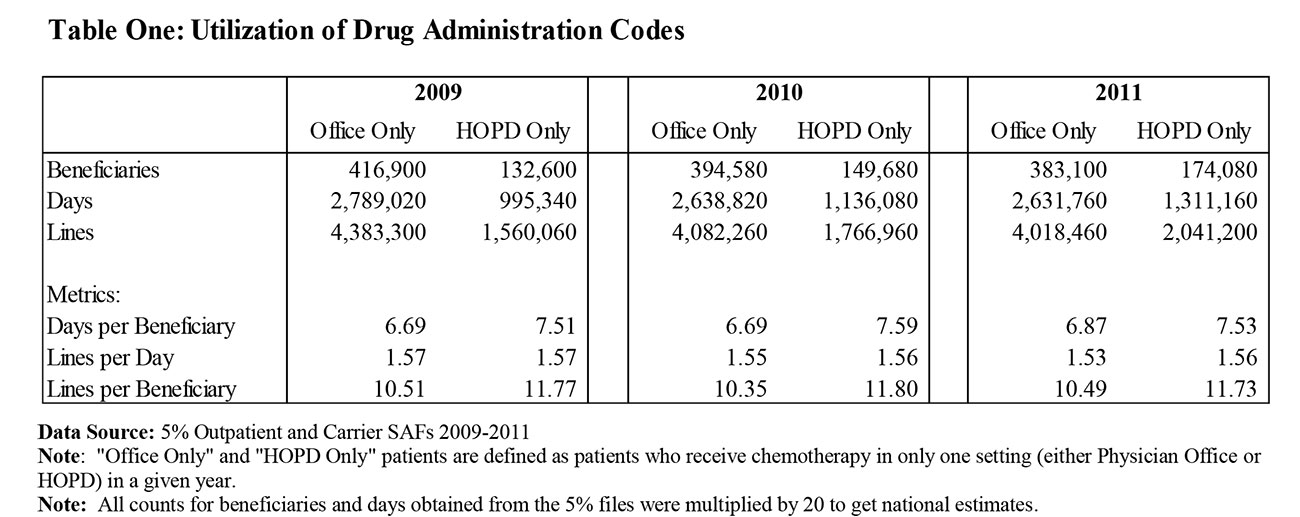
Table One provides the data underlying the comparisons in Figure 1
We do not present a similar comparison of utilization trends between the HOPD and Office for chemotherapy drugs because low-cost chemotherapy drugs may not be separately paid in the HOPD due to packaging under the OPPS payment system, while being paid in the Office setting. This leads to biased volume trends when we compare utilization in the form of paid drug lines between the two settings.
Illustrative Overview: Spending on Drugs and Chemotherapy Administration
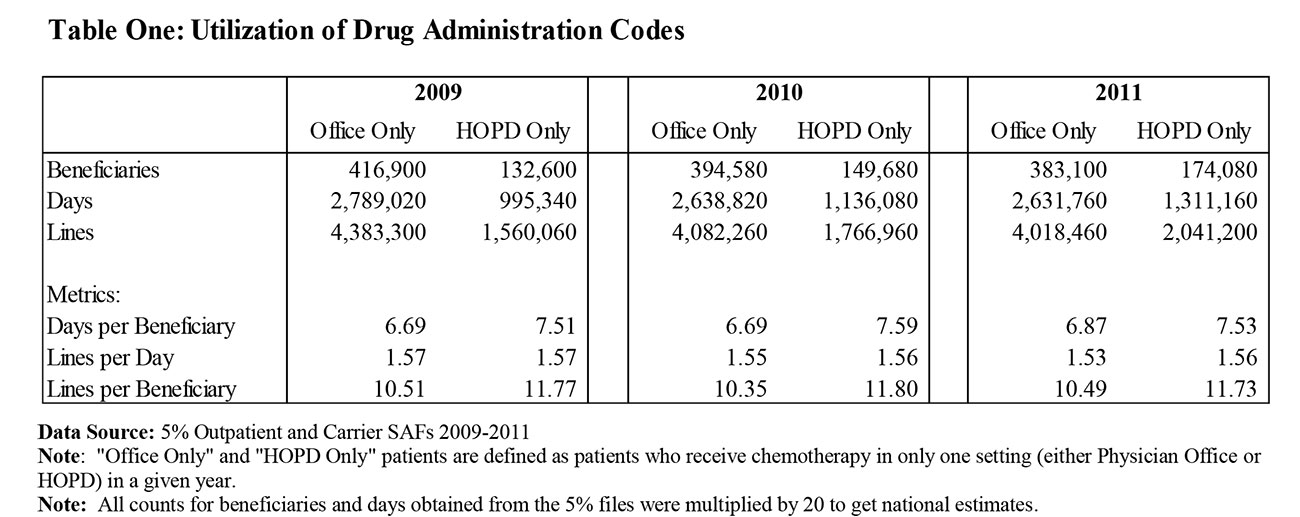
After comparing service volumes across settings, we move to a comparison of spending on chemotherapy administration, as well as separately paid drugs and biologicals. Figure 2 below shows that across the three years of data, chemotherapy administration payments per unit of utilization in HOPD Only patients have been higher than Office Only patients.
As shown in that figure:
- On an annual basis, spending per beneficiary on chemotherapy administration in our samples is roughly 50% higher in the outpatient hospital than the office.
- Similar differentials exist when comparing administration payments per day and payments per line.
Again, the claims data available do not permit us to understand whether there are any case-mix differences in the populations served by these two settings or what impact on the results adjusting for any such differences would have, but we believe these comparisons illustrate the difference in spending between the two settings.
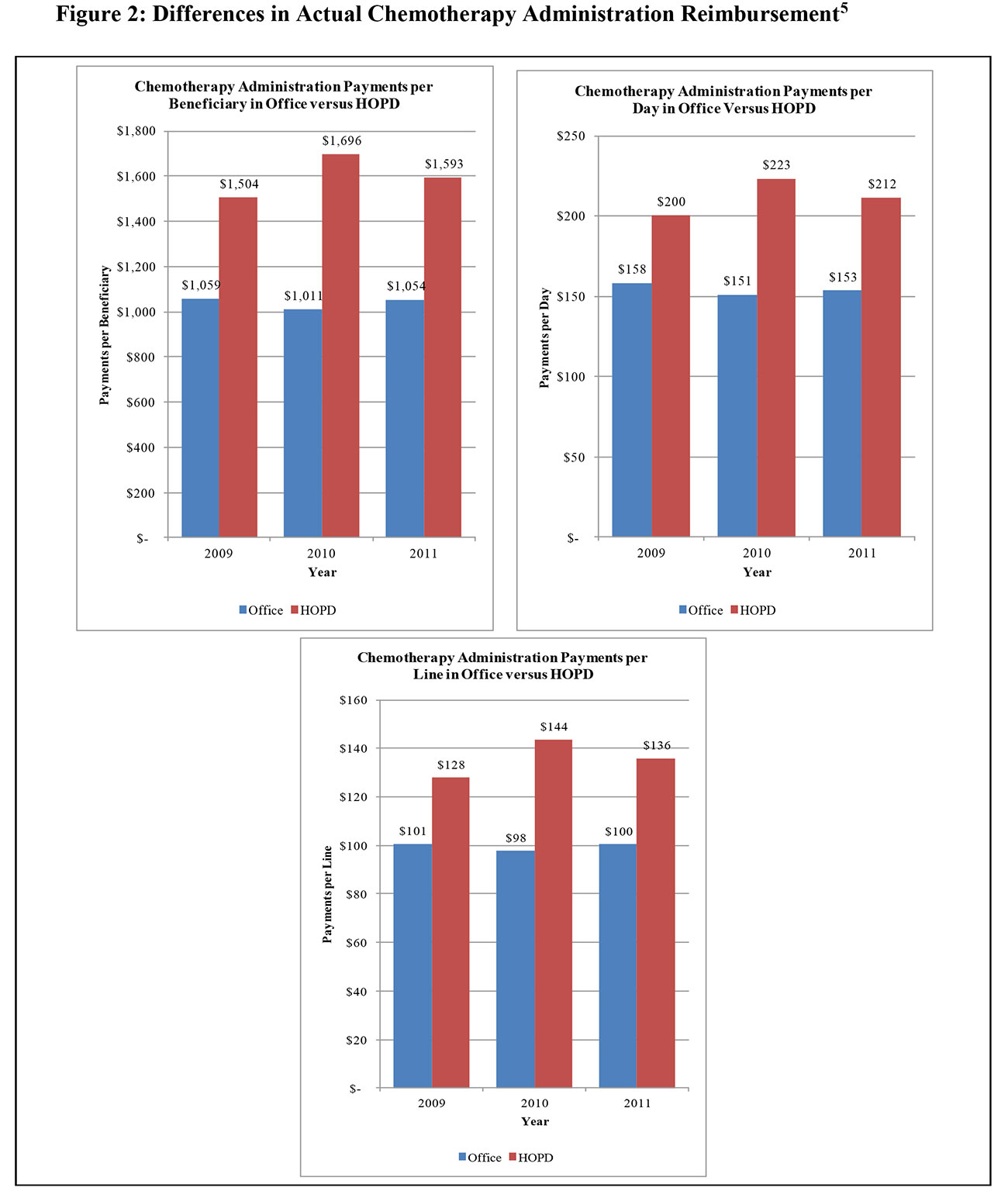
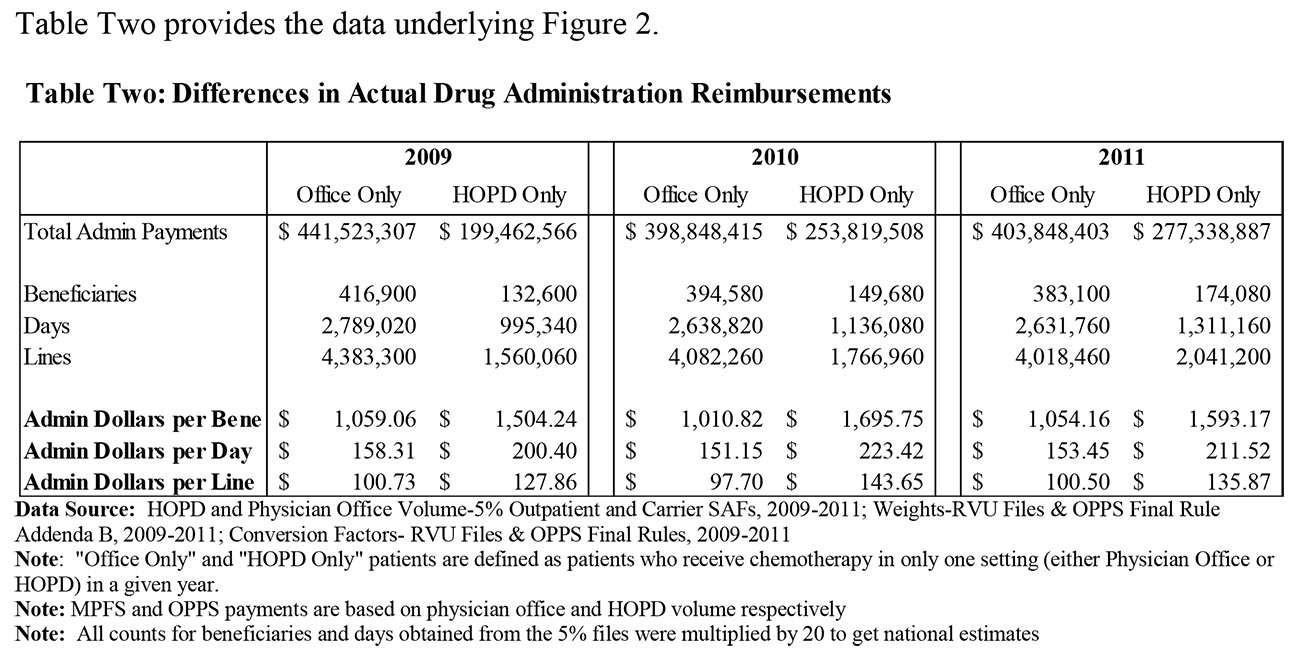
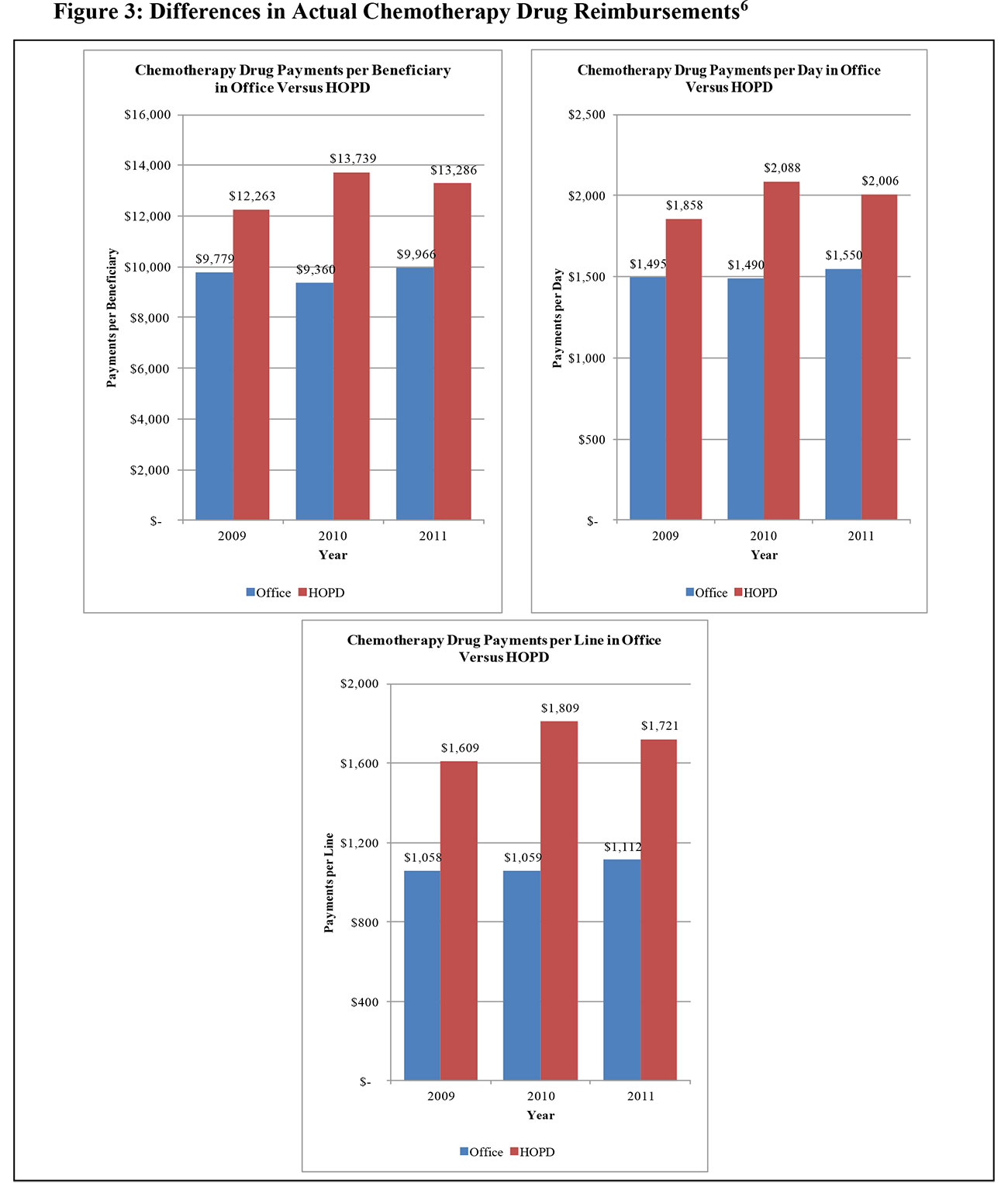
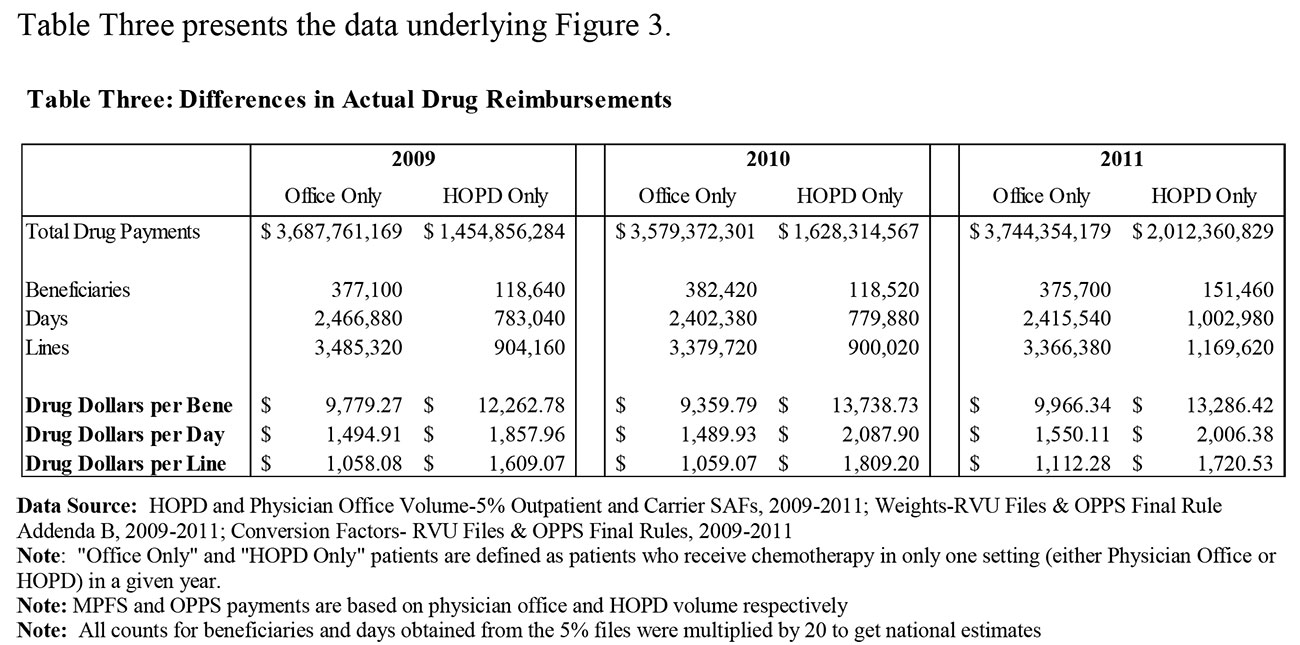
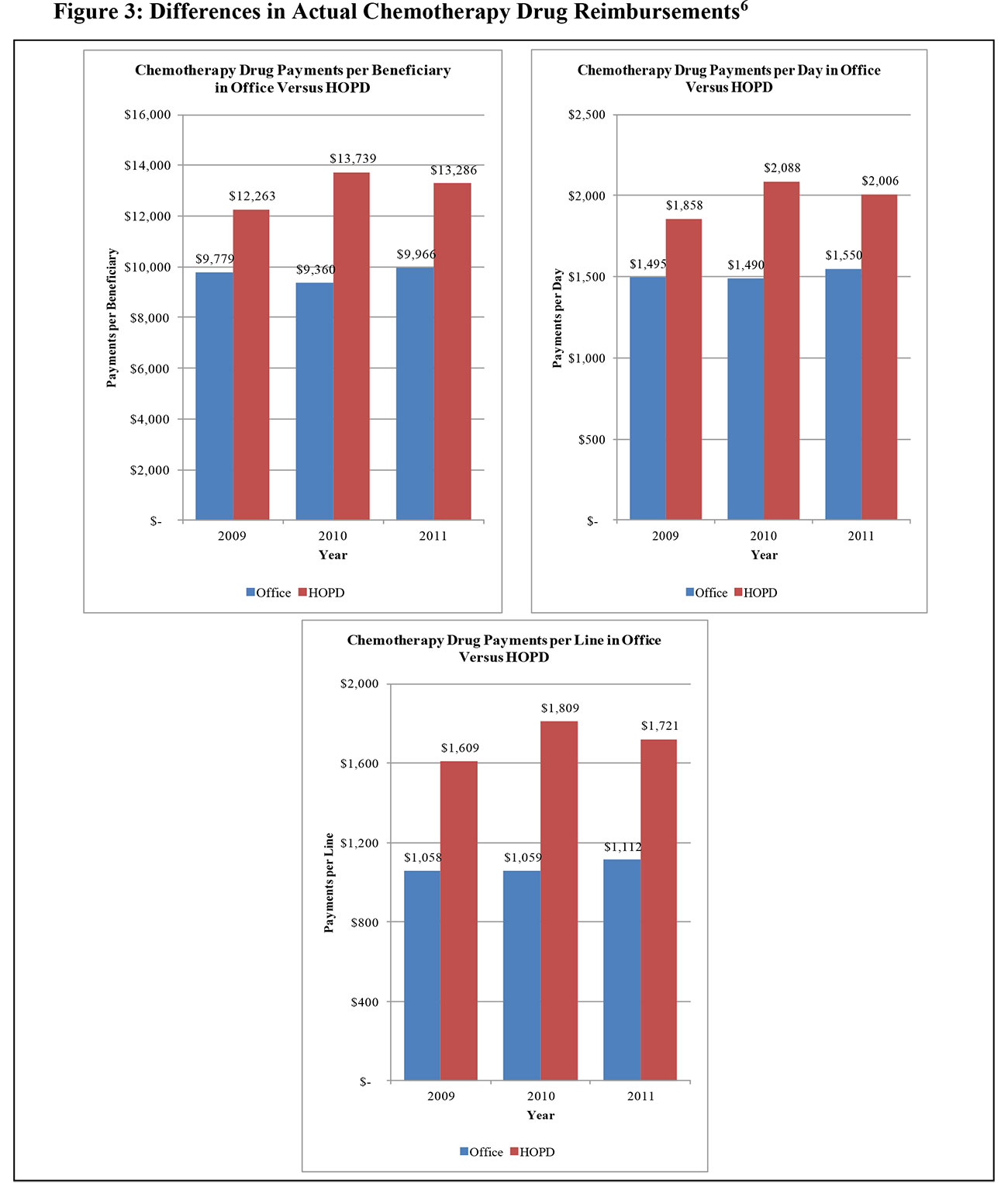
Figure 3 extends the reimbursement analysis to focus on separately reimbursed chemotherapy products used to treat patients in our sample.
As indicated in the figure, beneficiaries receiving their care only in hospitals received a total quantum of chemotherapy drugs that had a materially higher reimbursement value than did those who received their chemotherapy care only in the office.
The data in Figure 3 show that, throughout our period, Medicare spending for chemotherapy drugs per patient day was consistently higher in the HOPD Only group than in the Office Only group, despite lower payment rates for drugs during the period for HOPDs. During the period in question, the incremental drug spending per day in the outpatient setting ranges from 24-40% higher than the physician office. Throughout the period of our analysis, drugs were reimbursed at 106% of the manufacturer’s Average Sales Price (ASP) in the office setting. Reimbursements for separately-payable drugs under the OPPS, by contrast, were at either 104% or 105% of ASP in those years. In 2013, drugs are reimbursed at 106% of ASP in both settings. If the differences in drug utilization were to continue as observed in 2009-2011, the spending differential between the hospital outpatient and the office will be even larger in 2013.
As previously noted, we cannot tell using claims data whether this difference reflects higher case mix in the outpatient hospital setting—which could necessitate a more expensive mix of drugs— or regimen choices among competing alternatives that are made differently in the two settings. We attempted to determine whether there were marked differences in patient diagnostic presentations across settings, but found that we could not reach any clear conclusions relying solely on claims data. There is some suggestion in the data that the outpatient setting may have a meaningfully larger share of cases presenting with lower-frequency diagnoses, but we were unable, given the limitations of the data, to draw any conclusions regarding whether these apparent case mix differences actually explained some or all of the observed difference in drug costs.
Decomposing Reimbursement Differences Between Physician and Hospital Payments for Outpatient Chemotherapy
The unit payment rate differences noted in the comparisons above are rooted in the differences between the two payment systems. When chemotherapy services are rendered to patients in a physician’s office, payment is made under the MPFS. Separate payment is made for the drugs administered, and for the codes reported to reflect the mode of administration for the drugs.7 The practice expense relative values for these services are based on non-facility payment rates intended to reflect the higher costs physicians incur when services are rendered in a setting where the physician is responsible for furnishing the clinical labor, medical supplies and equipment necessary to perform the service.
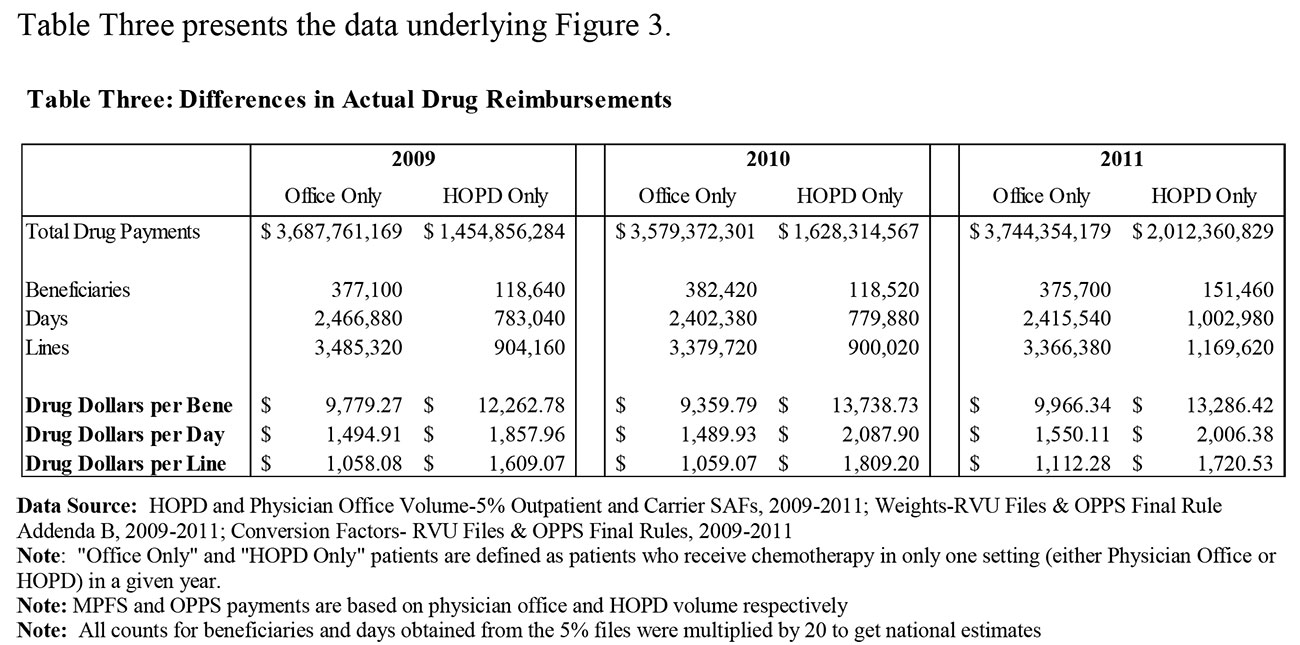
When chemotherapy services are rendered to patients in the outpatient hospital setting, the services are reimbursed under the OPPS. As in the office setting, many chemotherapy drugs are separately reimbursed in the outpatient hospital, though prior to 2013, the unit payment rates for drugs have tended to be slightly lower in the outpatient hospital than in the office setting.8 Payment for drug administration services is made based on the assignment of each chemotherapy administration code to an Ambulatory Payment Classification (APC). Under the OPPS, the 14 general and 8 specialized chemotherapy administration codes map to four discrete chemotherapy administration APCs. The valuation of these APCs is in no way related to the payment rates for any of these 22 services under the Fee Schedule. Rather, it is based on analysis of hospital cost data imputed to claims for these services rendered in the hospital. Hence, there is significant variation in the cost to the Medicare program for these services depending on the setting of care. Table Four shows a comparison of national allowed payment rates across sites.
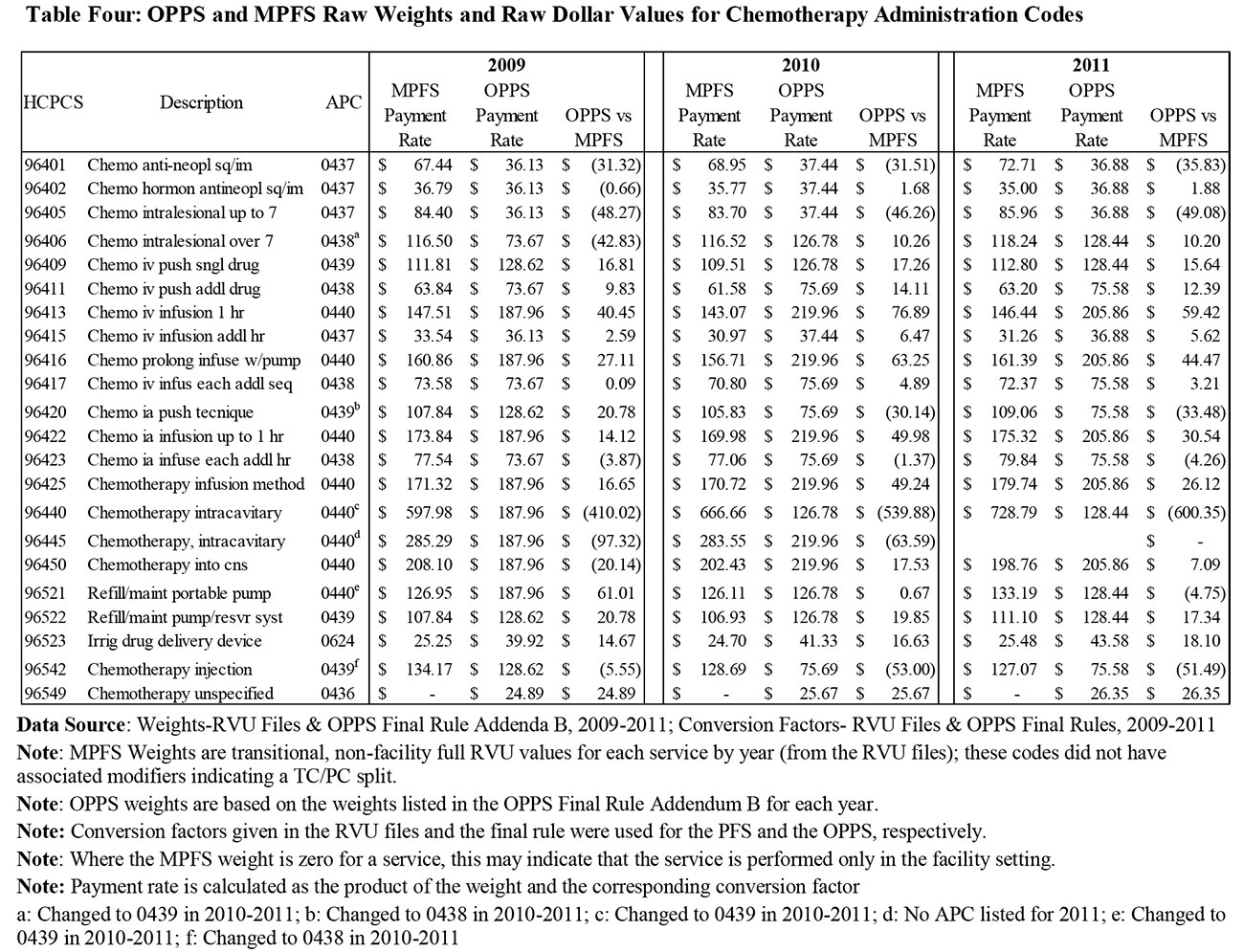
As indicated in the table, the drug administration codes paid in the outpatient hospital are, for a majority of the codes payable under the Fee Schedule, higher under the OPPS than under the MPFS in the office setting. In 2009, 12 of the 21 codes payable in both setting were higher in the OPPS. In 2010 and 2011, the number of codes with higher payments in the OPPS rises to 15 and 14 codes respectively.
As this presentation makes clear, the contribution of payment rate differentials to cross-site payment differences cannot be gauged solely by look at nominal payment rates.
Measurement of Cost Differences Between OPPS and MPFS Chemo Payments
The analysis we present in this report reflects our view that there is no “best” single measure of the differences in costs Medicare incurs when patients are treated in one setting or another.9
As will be discussed more fully below, the differences in payment methodologies across these two payment settings are multi-dimensional. The major differences include:
- Differences in the granularity of the coding schemes used to classify services;
- Differences in the data used and the methodologies employed to calculate payment rates under each system for each code;
- Differences in the rate at which payments are updated under the MPFS versus the OPPS; and, to a lesser extent;
- Differences in the way beneficiary cost sharing is determined—and hence differences in the share of the allowed payment paid by the Medicare program.
There may also be differences in Medicare costs due to variations in the characteristics of patients treated in one setting versus another (that is, case mix), and differences in practice styles that may differentially affect the frequency or intensity of services rendered in one setting versus another. Our ability to evaluate these potential differences using administrative claims data is limited. While we have employed claims data to take a high level look at the possibility of case mix differences, we cannot reach robust conclusions about the import of such “behavioral” differences across settings given the data available. For this reason, we have focused our analysis on chemotherapy services, excluding other potential sources of cross-site payment differences, such as evaluation and management services and diagnostic testing, on the grounds that the rationale for the location of those services may be totally unrelated to the decision to render chemotherapy services in one setting or another.
For these reasons, the analysis we present is intended to help policymakers understand the relative importance of different determinants of cross site payment differentials for chemotherapy services.
A Volume-Weighted Rate Comparison
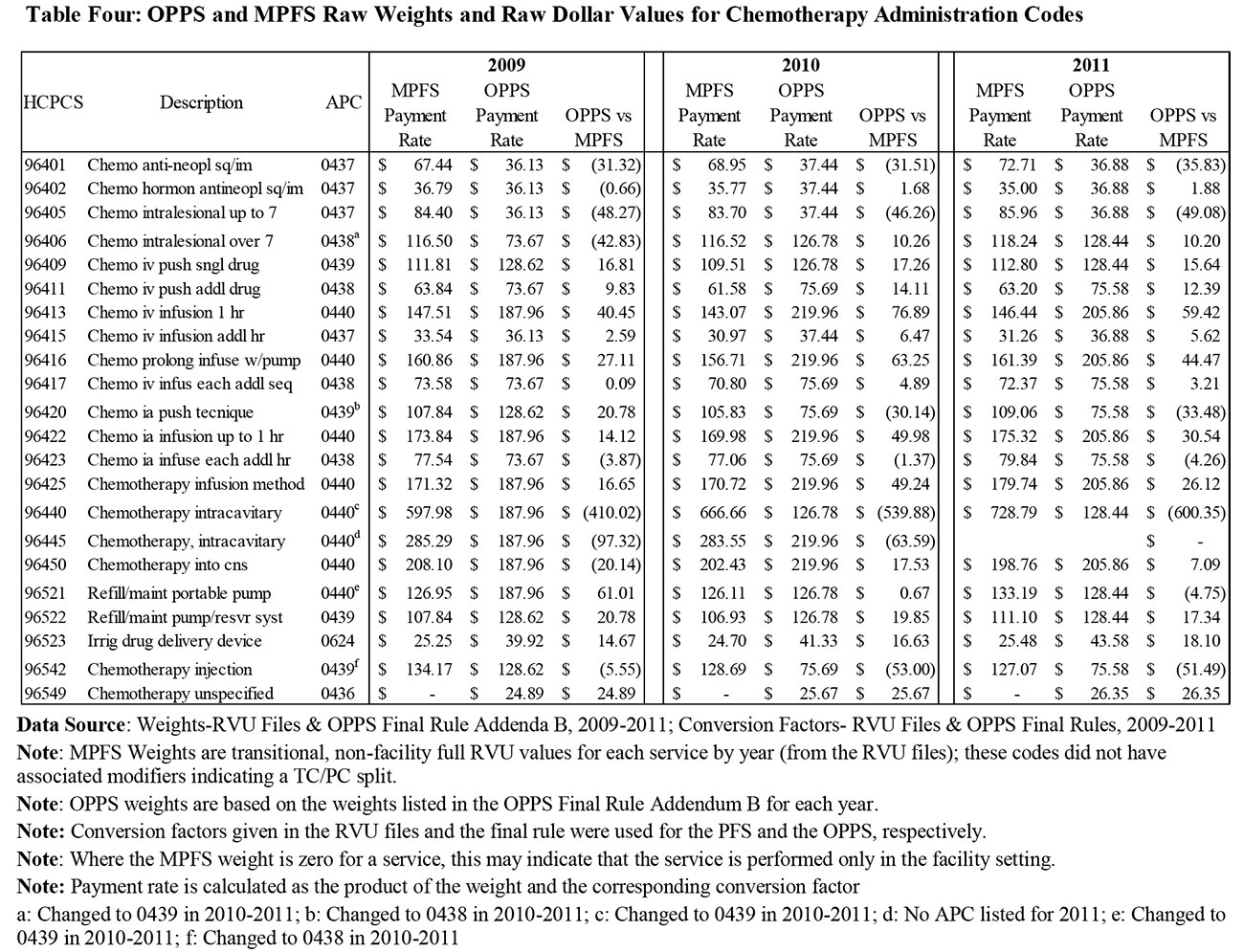
Table Five weights the payment rates for 2009-2011 by the volume of services rendered only in the office setting in each of those years. Thus, the data in Table Five provide a general indicator of how office-based services would “reprice” if cases being paid in those years under the office rates had instead been paid using that year’s OPPS rates.
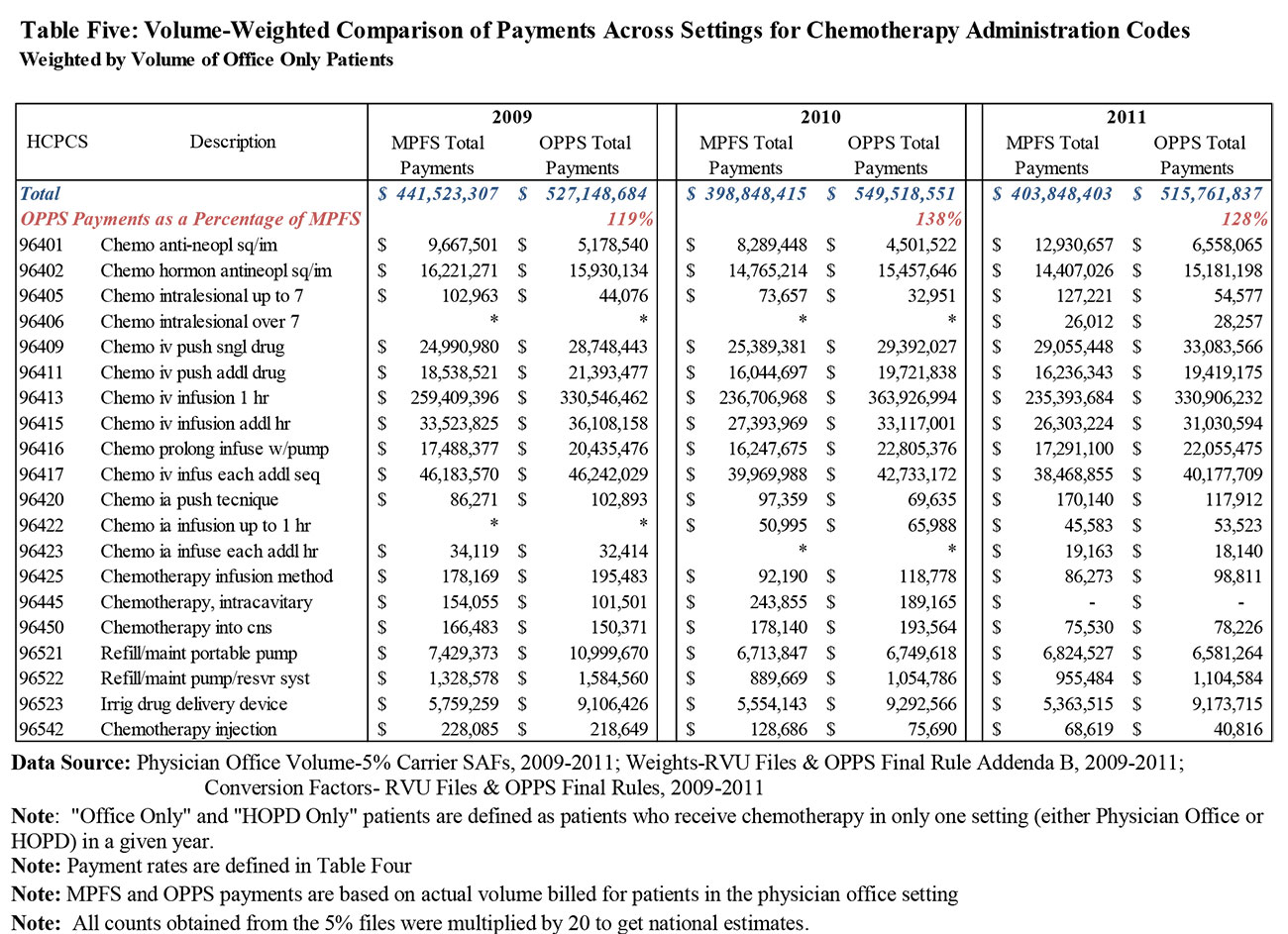
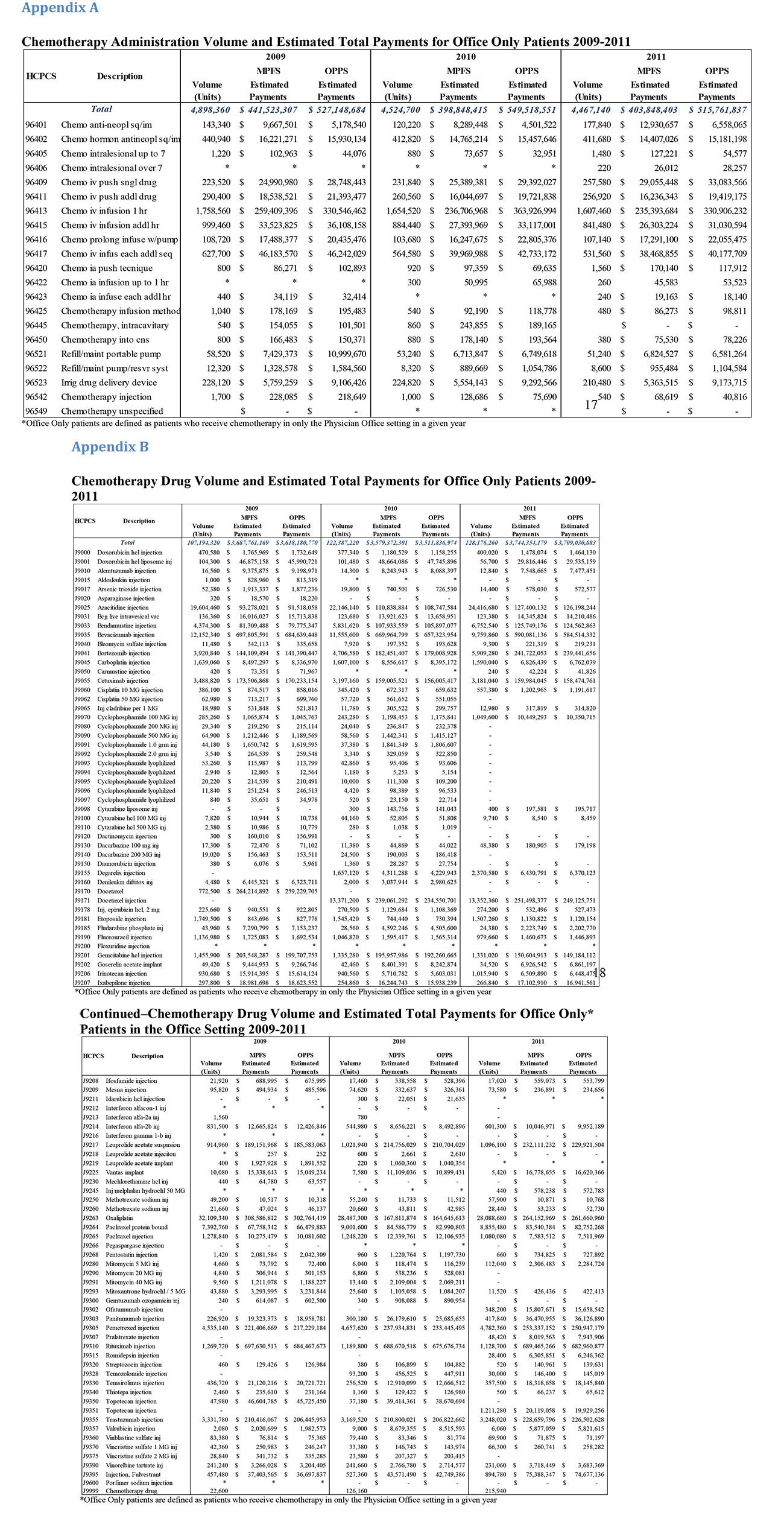
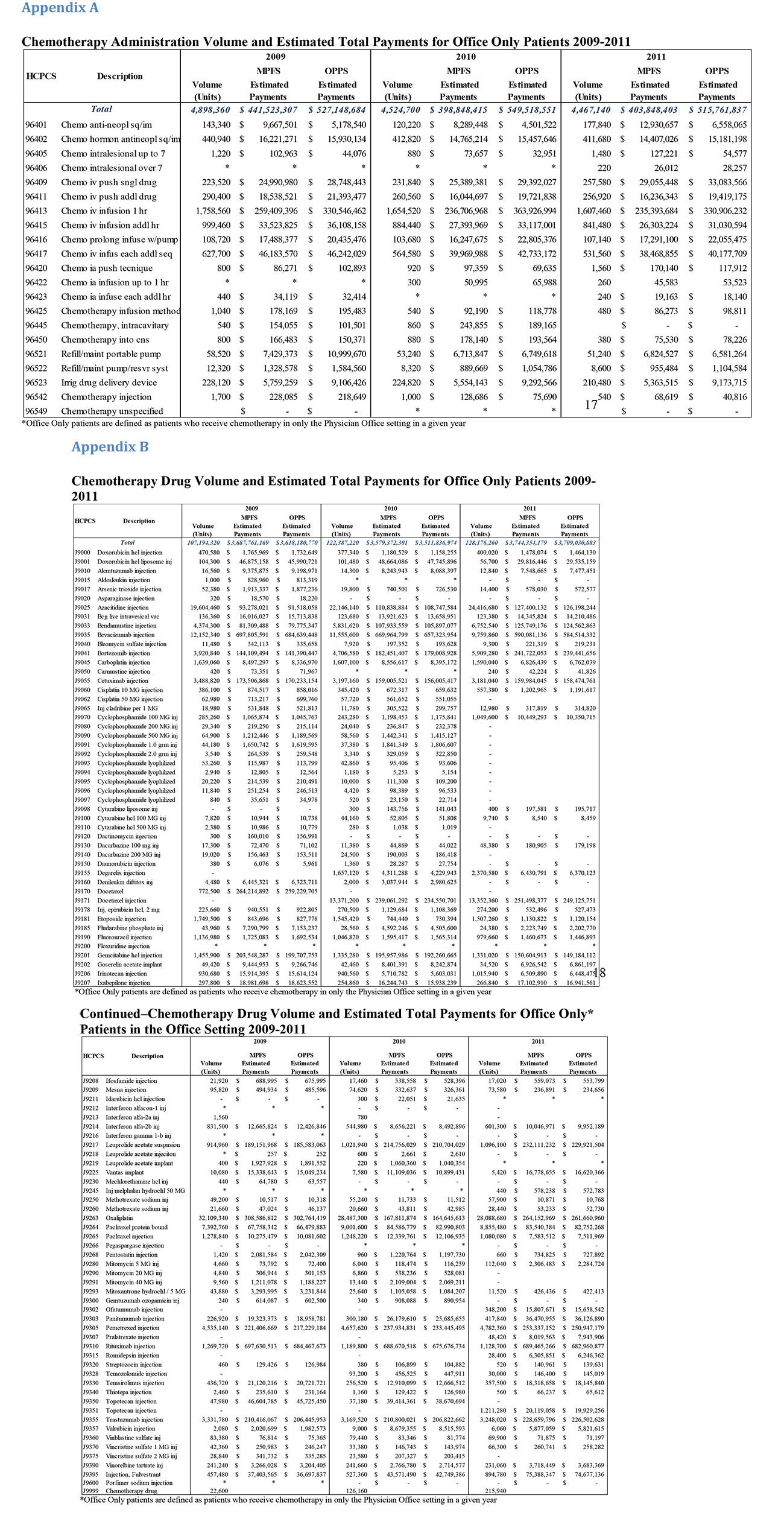
The volumes used to generate this comparison reflect utilization by Office Only patients— patients who, in the year in question, received chemotherapy services only in the office setting.10 Thus, these estimates reflect the pure effect of payment differentials between office-based care and hospital-based care for these patients. As these data indicate, re-pricing these office cases to OPPS payment rates creates a volume-weighted payment differential of 19-38% in the years under study. As may be inferred from these estimates, significant cross-site pricing differentials for the highest-volume drug administration techniques explain most of the difference in these estimates. The volume and pricing detail underlying this analysis is presented in Appendix A.
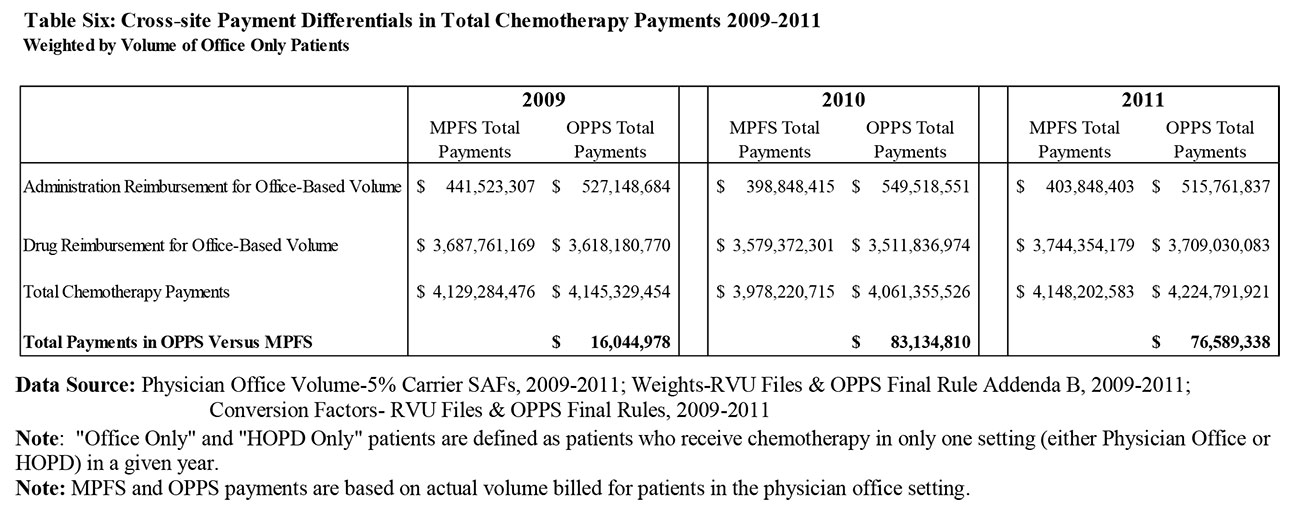
Table Six extends the analysis presented in Table Five to show the relative contribution of drug pricing differentials to disparities in chemotherapy payments across sites. It shows how the aggregate allowed payment differential shown in Table Five compares to allowed payments for drugs across both settings for Office Only patients. Adding drug costs into the analysis does materially narrow the gap in both dollar and percentage terms for prior years, but beginning in 2013, CMS equilibrated drug reimbursement in the HOPD with payments in the MPFS (for separately paid products). Policymakers seeking to extract rules of thumb from our analysis regarding the magnitude of cross-site payment differentials should be careful to take cognizance of the distinction between drug administration services and the cost of the drugs themselves. Detailed information about drug utilization by Office Only patients is available in Appendix B.
The Impact of Cost Sharing Differentials
As previously shown above, differences in drug utilization and payment rates for drug administration services are the main drivers of differences in Medicare payments for cancer care across settings. These differences in allowed payments are, however, mitigated modestly by the fact that patient cost sharing obligations are somewhat higher under the OPPS, and hence the share of the allowed payment paid for by the Medicare program is lower.11
Simply bringing cost sharing into the equation lowers our estimates of Medicare payments in both settings due to the fact that beneficiaries pay out of pocket roughly one-fifth of total costs. Based on our estimates, beneficiary cost sharing differences for drug administration services narrow the spread between OPPS payments and MPFS payments by only 0.2%.
Differences Attributable to Different Update Policies
As suggested above, part of the observed disparity in payments based on alternative payment methods results from the fact that the update policies applied in the MPFS and the OPPS, while conceptually similar, result in materially different updates from year to year.
Under the OPPS, the annual update in the conversion factor is anchored off a projection of the likely rate of increase in hospital input costs, as measured against a market basket of goods and services typically purchased by hospitals. While further adjustments are then made to recoup productivity increases and other policy adjustments that Congress imposes from time to time, the OPPS system typically receives a meaningful positive update each year.
Under the MPFS, the annual update to the conversion factor is anchored off a “Medical Economic Index” (MEI) projection that is quite similar in concept to the hospital market basket index. Unlike the OPPS system, however, permissible updates are constrained by a formula that offsets payments to recoup increases in service volume relative to permissible growth targets.12 Over the last decade, payment reductions resulting from automatic application of this formula would have been quite drastic, motivating policymakers to override the formula in favor of payment freezes or modest increases.
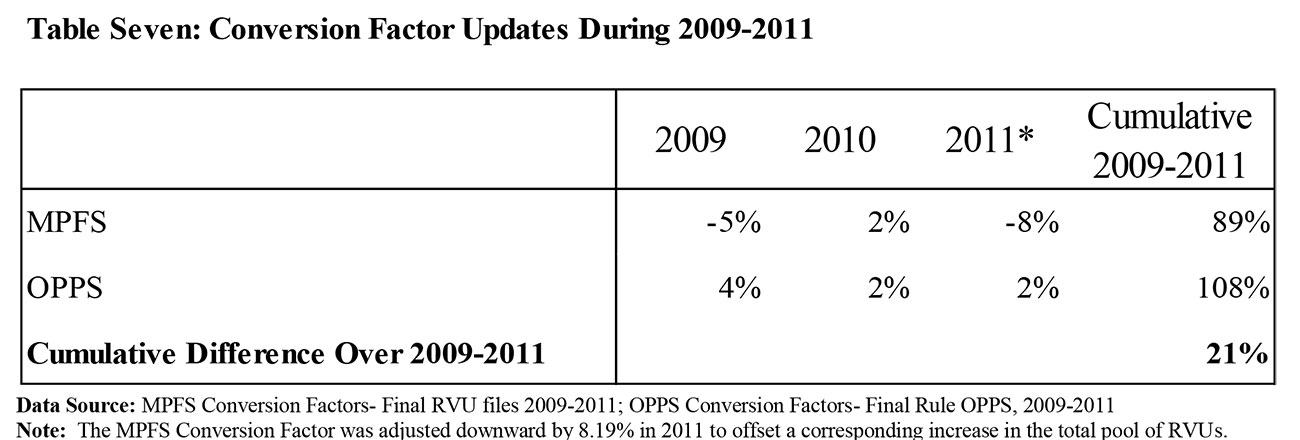
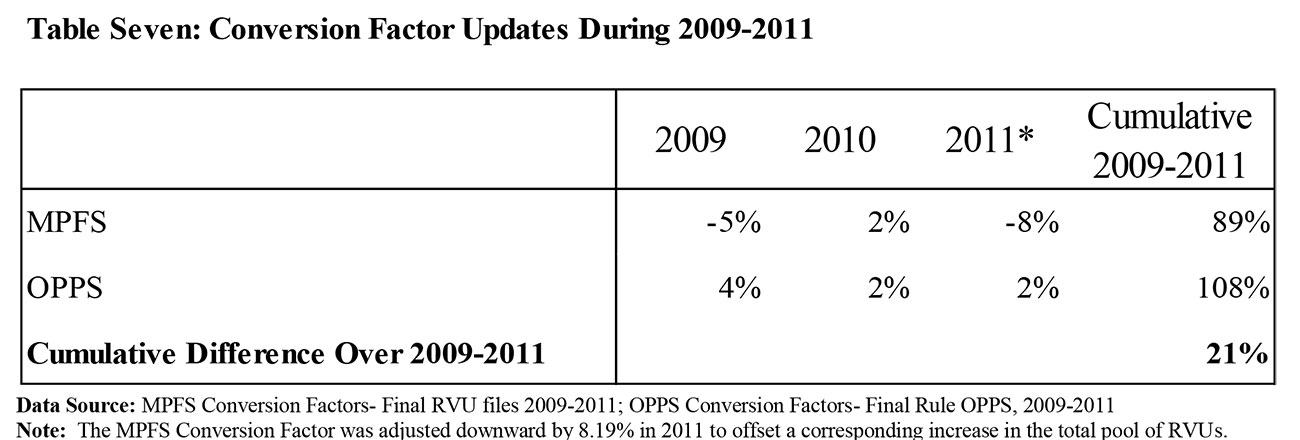
As a result of these disparities in method of establishing update percentages, there has been a growing gap between the conversion factors in favor of the OPPS system. Because these disparities are cumulative over time, estimates of the effect of the conversion factor divergence will vary depending on the time interval analyzed. The dollar values presented in Tables Five and Six embed the conversion factor update disparities that actually occurred over the 2009-2011 period.13 Table Seven shows the actual conversion factor updates applied to payments under both systems.
Conclusions
In summary, we find that:
- As discussed above, our comparison of service use rates across settings leads to the conclusion that patients receive more chemotherapy administrations on average when treated in the outpatient hospital, and that the dollar value of chemotherapy agents used is meaningfully higher in the outpatient hospital.
- Payment rate differentials across Medicare payment methodologies make chemotherapy administration more costly, on a unit price basis, in the hospital outpatient setting.
- During the period of our analysis, a portion of this difference was mitigated by unit reimbursement rate differences for chemotherapy drugs. Going forward, however, the drug reimbursement differential has been eliminated.
- As a result, we expect payment rate disparities between services provided in the office setting and the hospital to grow over time as payment update differentials favoring the outpatient hospital setting widen.
- We also expect differences in overall spending per beneficiary between the office setting and hospital to grow over time now that drugs are paid at the same rate and the differential in services payments continues to widen.
- Using only claims data, however, we cannot measure the level of case mix differences between the two settings, or what impact adjusting for any such differences might have on our results.
1 “Results of Analyses for Chemotherapy Administration Utilization and Chemotherapy Drug Utilization, 2005- 2011 for Medicare Fee-for-Service Beneficiaries”, Moran Company Memorandum to The US Oncology Network, et al. (May 29, 2013).
2 In this project, we have restricted our analysis of payments to those associated with drugs and chemotherapy administration. In addition to receiving these services, providers of these services may also bill for office or clinic visits and diagnostic tests. For reasons that will be discussed more fully below, we have not analyzed differences in the frequency and cost with which these services are billed across settings.
3 While roughly half of this differential was offset by lower reimbursement for drugs in the OPPS over the period we studied, CMS began to pay for most chemotherapy agents at the same rates across settings in 2013.
4This analysis is intended to illustrate differences between the OPPS and MPFS, but does not account for case mix differences between settings.
5 This analysis is intended to illustrate differences between the OPPS and MPFS, but does not account for case mix differences between settings.
6 This analysis is intended to illustrate differences between the OPPS and MPFS, but does not account for case mix differences between settings.
7 Our analysis focuses on reimbursement for therapeutic cancer drugs. As in our prior analysis, we have not considered the volume or cost of “supportive care” drugs, e.g., anti-emetics, given to patients receiving chemotherapy in different settings.
8 Throughout the period of our analysis, drugs were reimbursed at 106% of the manufacturer’s Average Sales Price (ASP) in the office setting. Reimbursements for separately-payable drugs under the OPPS, by contrast, were at either 104% or 105% of ASP in those years. Not all drugs are, however, separately payable under the OPPS; drugs with per-day costs below a fixed threshold, presently $80 (and between $60 and $70 during the period of our analysis), are “packaged” into the APC payment rates. Our analysis of payment differentials takes account of these differences.
9 Many of the findings we present from our analysis of Medicare costs may be equally applicable to differences in costs incurred by other payers. Since we have restricted our analysis to the costs associated with Medicare patients under Medicare payment methodologies, however, we cannot reach that conclusion.
10 In our analysis, a patient who received only office-based chemotherapy in particular year may have had hospital-based chemotherapy in another year.
11 Prior to the implementation of the OPPS in 2000, beneficiary coinsurance was based on billed charges, which were typically higher than cost (the determinant, at that time, of allowed payments). The statute required the Secretary to implement a cost sharing amount for each APC that preserved that historical relationship until such time as a normal Part B cost sharing obligation of 20% of allowed payments exceeded the historical cost sharing amount.
12 This policy is commonly referred to as the “sustainable growth rate (SGR)” policy, the label given in the statute to the component of the formula that determines the target rate of increase.
13 We note that the conversion factor update differential applies only to payments for drug administration services: the SGR policy has no effect on the calculation of the ASP values on which reimbursements for separately-billed drugs are based.
Cost Differences in Cancer Care Across Settings
Cost Differences in Cancer Care Across Settings
In a prior memorandum, we presented evidence documenting the growing share of Medicare oncology volume being billed in the outpatient hospital setting, in comparison to the physician office setting.1 In this report, we present our assessment of the cost consequences to the Medicare program of patients receiving chemotherapy services in physician offices versus hospital outpatient departments on the basis of Medicare data from the years 2009-2011.
In performing this analysis, we have focused on cross-site spending and payment rate differentials that result from differences in the utilization of drugs and services in addition to methodologies employed by Medicare to set payment rates in these two settings.2
Highlights of Our Analyses:
- By a variety of metrics, estimated chemotherapy spending is higher under the Hospital Outpatient Prospective Payment system (OPPS) than corresponding payments in the physician office under the Medicare Physician Fee Schedule (MPFS) for the same set of patients despite lower unit payment rates for drugs in the OPPS during the 2009-2011 period.
- Our comparison of service use rates across settings leads to the conclusion that patients receive more chemotherapy administration sessions on average when treated in the outpatient hospital—and that the dollar value of chemotherapy services used is meaningfully higher in the outpatient hospital.
– Chemotherapy days per beneficiary were about 9 to 12 percent higher in the hospital outpatient department than the physician office setting across the 2009- 2011 period. The difference was 12.3% in 2009, 13.5% in 2010 and 9.6% in 2011.
– On a per beneficiary basis, hospital chemotherapy spending was approximately between 25 to 47 percent higher than physician office chemotherapy spending across the 2009-2011 period. The difference was 25.4% in 2009, 46.8% in 2010 and 33.3% in 2011.
– On a per chemotherapy day basis, hospital chemotherapy spending was 24.3% higher in 2009, 40.1% higher in 2010 and 29.4% higher in 2011 than physician office chemotherapy spending across the 2009-2011 period.
– On a per beneficiary basis, hospital chemotherapy administration spending was 42% higher in 2009, 67.8% higher in 2010 and 51.1% higher in 2011 than physician office chemotherapy administration spending.
- Using only claims data, we cannot determine the extent to which these differences in utilization reflected differences in patient case mix versus differences in facility practice style.
- Re-pricing office chemotherapy administration services using OPPS payment rates creates a volume-weighted payment differential of 19-38% over the 2009-2011 period of our analyses.3 In other words, if all physician office chemotherapy administration services had been paid using OPPS payment rates over the 2009-2011 period, Medicare would have paid 19-38% more for these services.
- Our analysis suggests that a significant portion of the difference in payment rates for chemotherapy administration services between the two sites of service can be attributed to the differing policies adopted by the Congress and CMS that set mechanisms by which OPPS and MPFS payments are updated.
The balance of this report provides further background and details about these conclusions, and the methodology underlying our analyses.
Differences in Utilization and Spending on Cancer Care Between the Hospital Outpatient Department and the Physician Office
In order to conduct a comparison of the treatment of cancer patients in the OPPS versus the physician office setting, we created a sample of Medicare claims for patients receiving chemotherapy in the year of analysis only in the outpatient hospital (“HOPD Only”) or only in the physician office setting (“Office Only”). The creation of this sample involved the omission of all cancer patients who received chemotherapy in both the Office and HOPD settings in the same year (4.2% of the prior sample). In addition to observing differences in payment rates across settings, we evaluated whether usage patterns differed depending on where patients received chemotherapy. Our analysis derives from a comparison of usage patterns of these two sub-populations.
While we see material differences in use patterns across the office versus the hospital setting, it is important to note that our analysis of claims data does not permit us to parse why usage patterns differ as they do. In particular, we cannot measure any differences associated with beneficiary characteristics (e.g., case mix) or what effects any such differences might have on utilization or spending. In addition, we are aware of anecdotal evidence of transitions from office-based cancer care to hospital outpatient-based cancer care over the past several years based on the acquisition of physician practices by hospital systems. In the case of such an acquisition, there could be a shift from the physician office to the outpatient hospital simply as a consequence of the acquisition, with no differences in patient population.
Illustrative Overview: Service Volumes
The figure that follows compares utilization between the HOPD and physician office for the average beneficiary in our HOPD Only and Office Only samples of Medicare claims
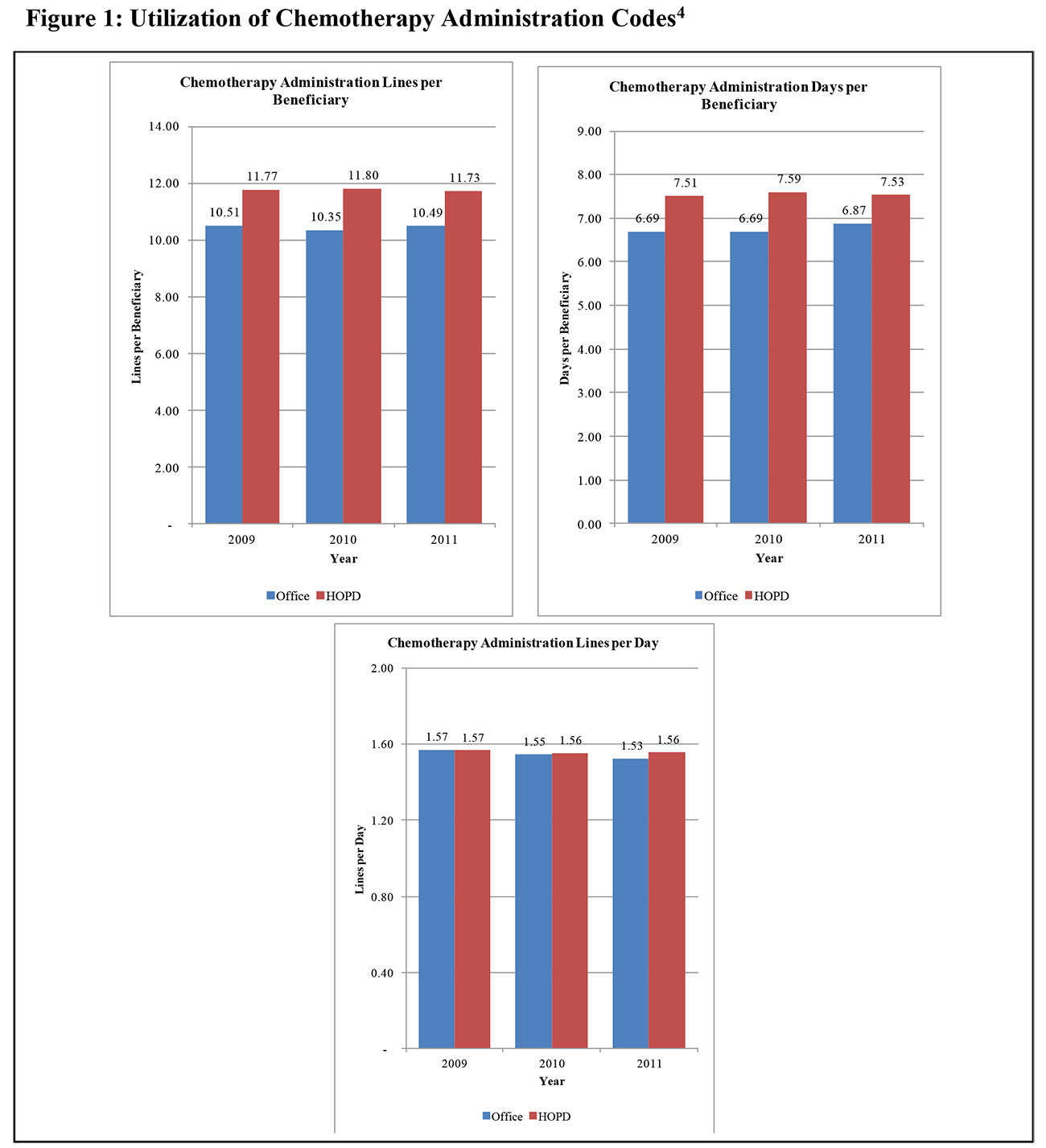
As shown in Figure 1, our comparison of chemotherapy use by Office Only and HOPD Only beneficiaries in these two discrete settings begins with an analysis of the frequency of drug administrations. The figure shows three separate illustrative comparisons:
- These data suggest that the HOPD Only population receives, throughout our period, about one additional day per year of treatment, relative to the days per year observed in the Office Only population.
- The observed difference in chemotherapy administration claim lines per beneficiary further reflects the greater frequency of care received by HOPD only patients.
- However, when we look at the number of discrete drug administration codes billed per day, as measured by the number of discrete service lines recorded on the claims, our data suggest that there may not be a material difference in the number of drug administration codes billed per day of care across settings.
Taken together, these data suggest that, in our period, HOPD Only chemotherapy patients received about a 10-13% higher frequency of drug administration than did Office Only patients. Given the trend pattern, it is unclear whether this spread would be expected to narrow or widen going forward.
Table One provides the data underlying the comparisons in Figure 1
We do not present a similar comparison of utilization trends between the HOPD and Office for chemotherapy drugs because low-cost chemotherapy drugs may not be separately paid in the HOPD due to packaging under the OPPS payment system, while being paid in the Office setting. This leads to biased volume trends when we compare utilization in the form of paid drug lines between the two settings.
Illustrative Overview: Spending on Drugs and Chemotherapy Administration
After comparing service volumes across settings, we move to a comparison of spending on chemotherapy administration, as well as separately paid drugs and biologicals. Figure 2 below shows that across the three years of data, chemotherapy administration payments per unit of utilization in HOPD Only patients have been higher than Office Only patients.
As shown in that figure:
- On an annual basis, spending per beneficiary on chemotherapy administration in our samples is roughly 50% higher in the outpatient hospital than the office.
- Similar differentials exist when comparing administration payments per day and payments per line.
Again, the claims data available do not permit us to understand whether there are any case-mix differences in the populations served by these two settings or what impact on the results adjusting for any such differences would have, but we believe these comparisons illustrate the difference in spending between the two settings.
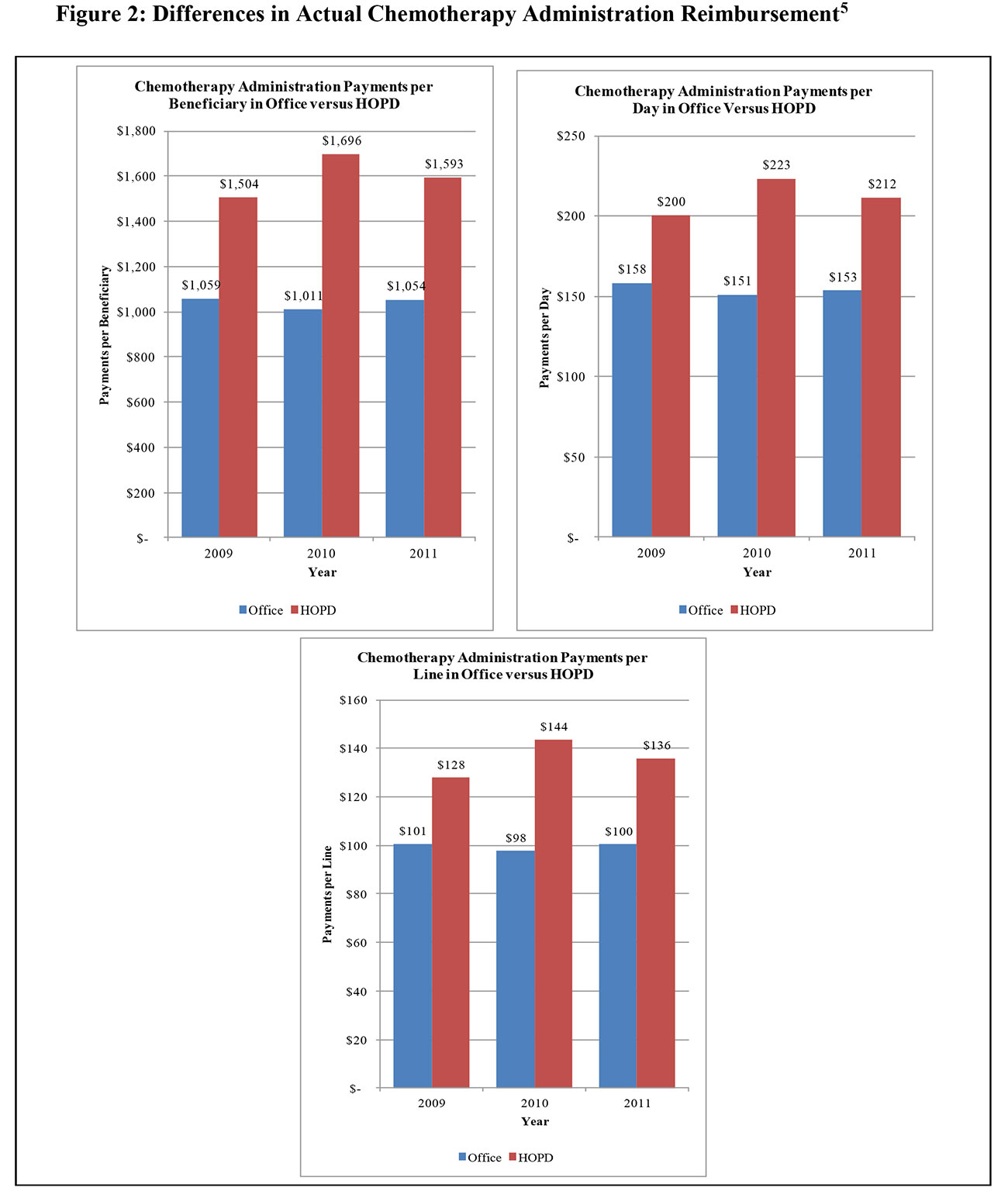
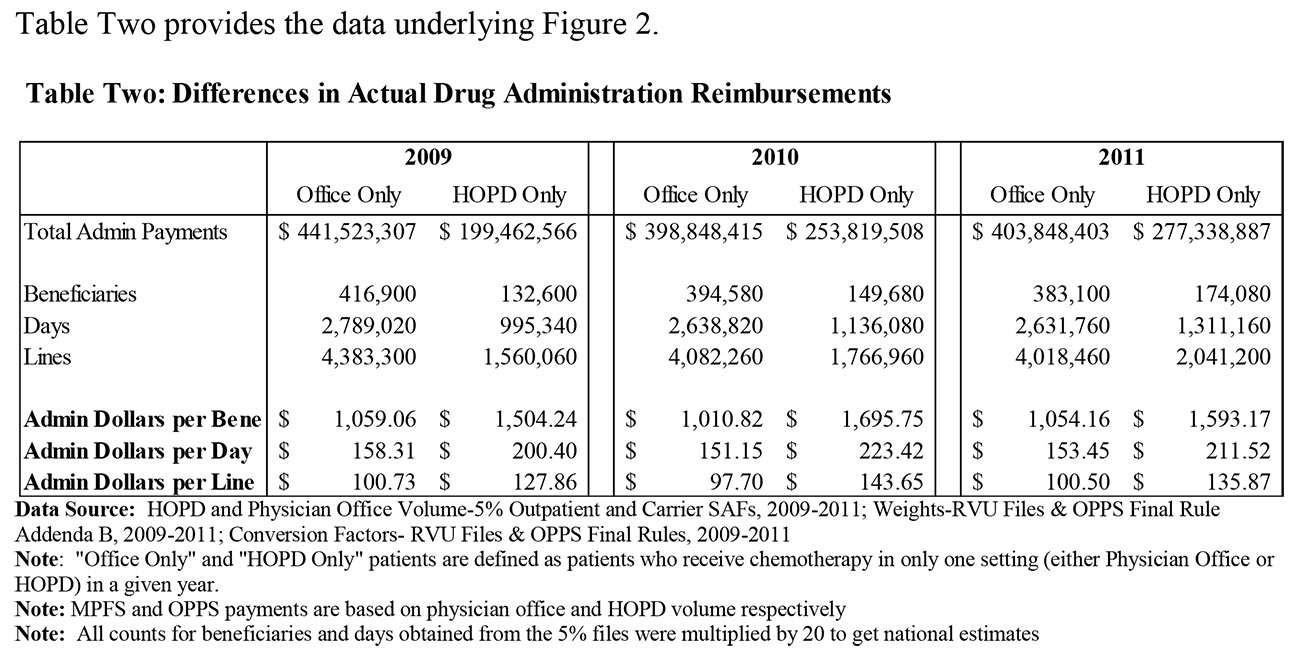
Figure 3 extends the reimbursement analysis to focus on separately reimbursed chemotherapy products used to treat patients in our sample.
As indicated in the figure, beneficiaries receiving their care only in hospitals received a total quantum of chemotherapy drugs that had a materially higher reimbursement value than did those who received their chemotherapy care only in the office.
The data in Figure 3 show that, throughout our period, Medicare spending for chemotherapy drugs per patient day was consistently higher in the HOPD Only group than in the Office Only group, despite lower payment rates for drugs during the period for HOPDs. During the period in question, the incremental drug spending per day in the outpatient setting ranges from 24-40% higher than the physician office. Throughout the period of our analysis, drugs were reimbursed at 106% of the manufacturer’s Average Sales Price (ASP) in the office setting. Reimbursements for separately-payable drugs under the OPPS, by contrast, were at either 104% or 105% of ASP in those years. In 2013, drugs are reimbursed at 106% of ASP in both settings. If the differences in drug utilization were to continue as observed in 2009-2011, the spending differential between the hospital outpatient and the office will be even larger in 2013.
As previously noted, we cannot tell using claims data whether this difference reflects higher case mix in the outpatient hospital setting—which could necessitate a more expensive mix of drugs— or regimen choices among competing alternatives that are made differently in the two settings. We attempted to determine whether there were marked differences in patient diagnostic presentations across settings, but found that we could not reach any clear conclusions relying solely on claims data. There is some suggestion in the data that the outpatient setting may have a meaningfully larger share of cases presenting with lower-frequency diagnoses, but we were unable, given the limitations of the data, to draw any conclusions regarding whether these apparent case mix differences actually explained some or all of the observed difference in drug costs.
Decomposing Reimbursement Differences Between Physician and Hospital Payments for Outpatient Chemotherapy
The unit payment rate differences noted in the comparisons above are rooted in the differences between the two payment systems. When chemotherapy services are rendered to patients in a physician’s office, payment is made under the MPFS. Separate payment is made for the drugs administered, and for the codes reported to reflect the mode of administration for the drugs.7 The practice expense relative values for these services are based on non-facility payment rates intended to reflect the higher costs physicians incur when services are rendered in a setting where the physician is responsible for furnishing the clinical labor, medical supplies and equipment necessary to perform the service.
When chemotherapy services are rendered to patients in the outpatient hospital setting, the services are reimbursed under the OPPS. As in the office setting, many chemotherapy drugs are separately reimbursed in the outpatient hospital, though prior to 2013, the unit payment rates for drugs have tended to be slightly lower in the outpatient hospital than in the office setting.8 Payment for drug administration services is made based on the assignment of each chemotherapy administration code to an Ambulatory Payment Classification (APC). Under the OPPS, the 14 general and 8 specialized chemotherapy administration codes map to four discrete chemotherapy administration APCs. The valuation of these APCs is in no way related to the payment rates for any of these 22 services under the Fee Schedule. Rather, it is based on analysis of hospital cost data imputed to claims for these services rendered in the hospital. Hence, there is significant variation in the cost to the Medicare program for these services depending on the setting of care. Table Four shows a comparison of national allowed payment rates across sites.
As indicated in the table, the drug administration codes paid in the outpatient hospital are, for a majority of the codes payable under the Fee Schedule, higher under the OPPS than under the MPFS in the office setting. In 2009, 12 of the 21 codes payable in both setting were higher in the OPPS. In 2010 and 2011, the number of codes with higher payments in the OPPS rises to 15 and 14 codes respectively.
As this presentation makes clear, the contribution of payment rate differentials to cross-site payment differences cannot be gauged solely by look at nominal payment rates.
Measurement of Cost Differences Between OPPS and MPFS Chemo Payments
The analysis we present in this report reflects our view that there is no “best” single measure of the differences in costs Medicare incurs when patients are treated in one setting or another.9
As will be discussed more fully below, the differences in payment methodologies across these two payment settings are multi-dimensional. The major differences include:
- Differences in the granularity of the coding schemes used to classify services;
- Differences in the data used and the methodologies employed to calculate payment rates under each system for each code;
- Differences in the rate at which payments are updated under the MPFS versus the OPPS; and, to a lesser extent;
- Differences in the way beneficiary cost sharing is determined—and hence differences in the share of the allowed payment paid by the Medicare program.
There may also be differences in Medicare costs due to variations in the characteristics of patients treated in one setting versus another (that is, case mix), and differences in practice styles that may differentially affect the frequency or intensity of services rendered in one setting versus another. Our ability to evaluate these potential differences using administrative claims data is limited. While we have employed claims data to take a high level look at the possibility of case mix differences, we cannot reach robust conclusions about the import of such “behavioral” differences across settings given the data available. For this reason, we have focused our analysis on chemotherapy services, excluding other potential sources of cross-site payment differences, such as evaluation and management services and diagnostic testing, on the grounds that the rationale for the location of those services may be totally unrelated to the decision to render chemotherapy services in one setting or another.
For these reasons, the analysis we present is intended to help policymakers understand the relative importance of different determinants of cross site payment differentials for chemotherapy services.
A Volume-Weighted Rate Comparison
Table Five weights the payment rates for 2009-2011 by the volume of services rendered only in the office setting in each of those years. Thus, the data in Table Five provide a general indicator of how office-based services would “reprice” if cases being paid in those years under the office rates had instead been paid using that year’s OPPS rates.
The volumes used to generate this comparison reflect utilization by Office Only patients— patients who, in the year in question, received chemotherapy services only in the office setting.10 Thus, these estimates reflect the pure effect of payment differentials between office-based care and hospital-based care for these patients. As these data indicate, re-pricing these office cases to OPPS payment rates creates a volume-weighted payment differential of 19-38% in the years under study. As may be inferred from these estimates, significant cross-site pricing differentials for the highest-volume drug administration techniques explain most of the difference in these estimates. The volume and pricing detail underlying this analysis is presented in Appendix A.
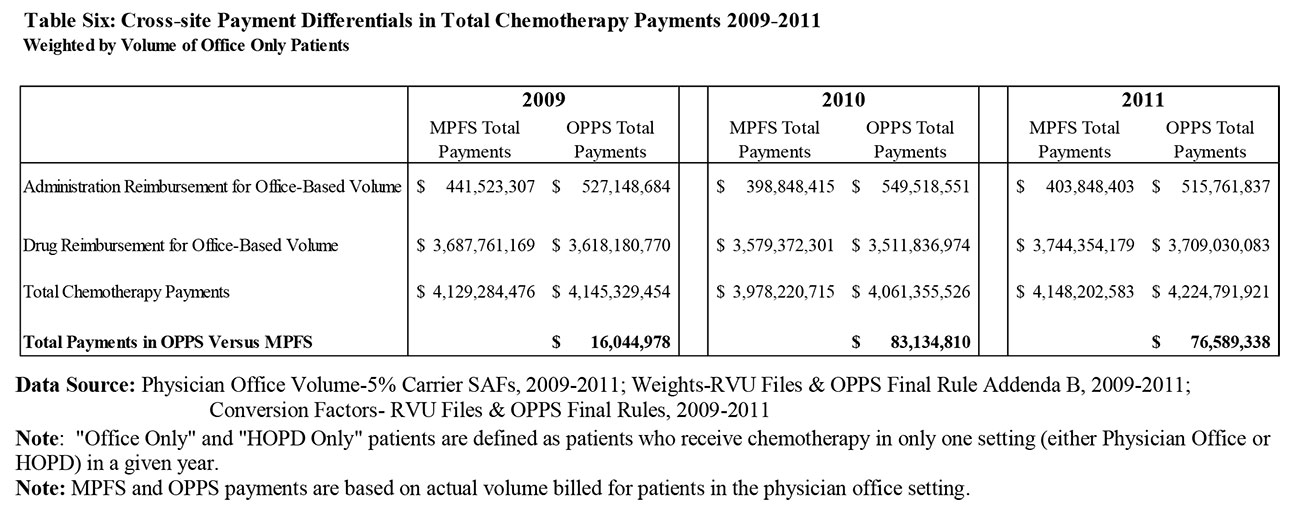
Table Six extends the analysis presented in Table Five to show the relative contribution of drug pricing differentials to disparities in chemotherapy payments across sites. It shows how the aggregate allowed payment differential shown in Table Five compares to allowed payments for drugs across both settings for Office Only patients. Adding drug costs into the analysis does materially narrow the gap in both dollar and percentage terms for prior years, but beginning in 2013, CMS equilibrated drug reimbursement in the HOPD with payments in the MPFS (for separately paid products). Policymakers seeking to extract rules of thumb from our analysis regarding the magnitude of cross-site payment differentials should be careful to take cognizance of the distinction between drug administration services and the cost of the drugs themselves. Detailed information about drug utilization by Office Only patients is available in Appendix B.
The Impact of Cost Sharing Differentials
As previously shown above, differences in drug utilization and payment rates for drug administration services are the main drivers of differences in Medicare payments for cancer care across settings. These differences in allowed payments are, however, mitigated modestly by the fact that patient cost sharing obligations are somewhat higher under the OPPS, and hence the share of the allowed payment paid for by the Medicare program is lower.11
Simply bringing cost sharing into the equation lowers our estimates of Medicare payments in both settings due to the fact that beneficiaries pay out of pocket roughly one-fifth of total costs. Based on our estimates, beneficiary cost sharing differences for drug administration services narrow the spread between OPPS payments and MPFS payments by only 0.2%.
Differences Attributable to Different Update Policies
As suggested above, part of the observed disparity in payments based on alternative payment methods results from the fact that the update policies applied in the MPFS and the OPPS, while conceptually similar, result in materially different updates from year to year.
Under the OPPS, the annual update in the conversion factor is anchored off a projection of the likely rate of increase in hospital input costs, as measured against a market basket of goods and services typically purchased by hospitals. While further adjustments are then made to recoup productivity increases and other policy adjustments that Congress imposes from time to time, the OPPS system typically receives a meaningful positive update each year.
Under the MPFS, the annual update to the conversion factor is anchored off a “Medical Economic Index” (MEI) projection that is quite similar in concept to the hospital market basket index. Unlike the OPPS system, however, permissible updates are constrained by a formula that offsets payments to recoup increases in service volume relative to permissible growth targets.12 Over the last decade, payment reductions resulting from automatic application of this formula would have been quite drastic, motivating policymakers to override the formula in favor of payment freezes or modest increases.
As a result of these disparities in method of establishing update percentages, there has been a growing gap between the conversion factors in favor of the OPPS system. Because these disparities are cumulative over time, estimates of the effect of the conversion factor divergence will vary depending on the time interval analyzed. The dollar values presented in Tables Five and Six embed the conversion factor update disparities that actually occurred over the 2009-2011 period.13 Table Seven shows the actual conversion factor updates applied to payments under both systems.
Conclusions
In summary, we find that:
- As discussed above, our comparison of service use rates across settings leads to the conclusion that patients receive more chemotherapy administrations on average when treated in the outpatient hospital, and that the dollar value of chemotherapy agents used is meaningfully higher in the outpatient hospital.
- Payment rate differentials across Medicare payment methodologies make chemotherapy administration more costly, on a unit price basis, in the hospital outpatient setting.
- During the period of our analysis, a portion of this difference was mitigated by unit reimbursement rate differences for chemotherapy drugs. Going forward, however, the drug reimbursement differential has been eliminated.
- As a result, we expect payment rate disparities between services provided in the office setting and the hospital to grow over time as payment update differentials favoring the outpatient hospital setting widen.
- We also expect differences in overall spending per beneficiary between the office setting and hospital to grow over time now that drugs are paid at the same rate and the differential in services payments continues to widen.
- Using only claims data, however, we cannot measure the level of case mix differences between the two settings, or what impact adjusting for any such differences might have on our results.
1 “Results of Analyses for Chemotherapy Administration Utilization and Chemotherapy Drug Utilization, 2005- 2011 for Medicare Fee-for-Service Beneficiaries”, Moran Company Memorandum to The US Oncology Network, et al. (May 29, 2013).
2 In this project, we have restricted our analysis of payments to those associated with drugs and chemotherapy administration. In addition to receiving these services, providers of these services may also bill for office or clinic visits and diagnostic tests. For reasons that will be discussed more fully below, we have not analyzed differences in the frequency and cost with which these services are billed across settings.
3 While roughly half of this differential was offset by lower reimbursement for drugs in the OPPS over the period we studied, CMS began to pay for most chemotherapy agents at the same rates across settings in 2013.
4This analysis is intended to illustrate differences between the OPPS and MPFS, but does not account for case mix differences between settings.
5 This analysis is intended to illustrate differences between the OPPS and MPFS, but does not account for case mix differences between settings.
6 This analysis is intended to illustrate differences between the OPPS and MPFS, but does not account for case mix differences between settings.
7 Our analysis focuses on reimbursement for therapeutic cancer drugs. As in our prior analysis, we have not considered the volume or cost of “supportive care” drugs, e.g., anti-emetics, given to patients receiving chemotherapy in different settings.
8 Throughout the period of our analysis, drugs were reimbursed at 106% of the manufacturer’s Average Sales Price (ASP) in the office setting. Reimbursements for separately-payable drugs under the OPPS, by contrast, were at either 104% or 105% of ASP in those years. Not all drugs are, however, separately payable under the OPPS; drugs with per-day costs below a fixed threshold, presently $80 (and between $60 and $70 during the period of our analysis), are “packaged” into the APC payment rates. Our analysis of payment differentials takes account of these differences.
9 Many of the findings we present from our analysis of Medicare costs may be equally applicable to differences in costs incurred by other payers. Since we have restricted our analysis to the costs associated with Medicare patients under Medicare payment methodologies, however, we cannot reach that conclusion.
10 In our analysis, a patient who received only office-based chemotherapy in particular year may have had hospital-based chemotherapy in another year.
11 Prior to the implementation of the OPPS in 2000, beneficiary coinsurance was based on billed charges, which were typically higher than cost (the determinant, at that time, of allowed payments). The statute required the Secretary to implement a cost sharing amount for each APC that preserved that historical relationship until such time as a normal Part B cost sharing obligation of 20% of allowed payments exceeded the historical cost sharing amount.
12 This policy is commonly referred to as the “sustainable growth rate (SGR)” policy, the label given in the statute to the component of the formula that determines the target rate of increase.
13 We note that the conversion factor update differential applies only to payments for drug administration services: the SGR policy has no effect on the calculation of the ASP values on which reimbursements for separately-billed drugs are based.